Abstract
Background: Paralytic ileus is a serious postoperative complication among individuals with colorectal cancer (CRC). Although mortality trends for CRC and paralytic ileus have been described separately, long-term national patterns involving both conditions have not been examined.
Methods: We analyzed U.S. mortality data for adults aged ≥45 years from 1999–2023 using CDC WONDER Multiple Cause-of-Death records. CRC was identified using ICD-10 codes C18–C20, and paralytic ileus using K56.0 and K56.7. Age-adjusted mortality rates (AAMRs) were calculated and standardized to the 2000 U.S. population. Joinpoint regression estimated annual percent change (APC) and average annual percent change (AAPC). Subgroup analyses were descriptive; formal between-group slope comparisons were not performed.
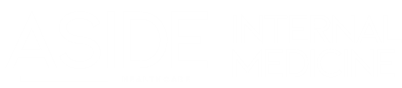
Results: A total of 31,363 deaths involved both CRC and paralytic ileus. The national AAMR declined from 1.48 per 100,000 in 1999 to 1.00 in 2023 (AAPC –1.50%; 95% CI –1.73 to –1.28). A significant decline occurred through 2012 (APC =– 3.27%), followed by a nonsignificant upward trend thereafter (APC = 0.63%; p = 0.057). Declines varied by sex, age group, race/ethnicity, and region, with the largest reductions among adults ≥65 years and in the Northeast. Most deaths occurred in inpatient settings (56%).
Conclusion: Mortality involving CRC and paralytic ileus declined substantially through 2012, then plateaued. Rising mortality among adults aged 45–64 years and persistent racial and geographic disparities highlight opportunities for improved perioperative quality initiatives, ERAS implementation, and opioid-sparing strategies.
References
1. Smith RET, Renaud RC, Hoffman E. Colorectal cancer market. Nat Rev Drug Discov. 2004: 471
2. Siegel RL, Miller KD, Jemal A. Cancer statistics. 2018 CA Cancer J Clin. 2018: 7
3. Granados-Romero JJ, Valderrama-Treviño AI, Contreras-Flores EH, Barrera-Mera B, Herrera Enríquez M, Uriarte-Ruíz K, Others. Colorectal cancer: a review. Int J Res Med Sci. 2017: 4667
4. Schwarz NT, Beer-Stolz D, Simmons RL, Bauer AJ. Pathogenesis of Paralytic Ileus. Ann Surg. 2002: 31
5. Weledji EP. Perspectives on paralytic ileus. Acute Medicine & Surgery. 2020:
6. Harnsberger C, Maykel J, Alavi K. Postoperative Ileus. Clin Colon Rectal Surg. 2019: 166
7. Chapuis PH, Bokey L, Keshava A, Mjfx R, Stewart P, Young CJ, Others. Risk Factors for Prolonged Ileus After Resection of Colorectal Cancer. Ann Surg. 2013: 909
8. Millán M, Biondo S, Fraccalvieri D, Frago R, Golda T, Kreisler E. Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J Surg. 2012: 179 https://doi.org/10.1007/s00268-011-1339-5]
9. Ju H, Shen K, Li J, Feng Y. Total postoperative opioid dose is an independent risk factor for prolonged postoperative ileus after laparoscopic colorectal surgery: a case-control study. Korean J Anesthesiol. 2024: 133
10. Chapuis PH, Bokey L, Keshava A, Mjfx R, Stewart P, Young CJ, Others. Risk factors for prolonged ileus after resection of colorectal cancer: an observational study of 2400 consecutive patients. Ann Surg. 2013: 909 https://doi.org/10.1097/SLA.0b013e318268a693]
11. Grigorean VT, Erchid A, Coman IS, Colorectal LeM. Cancer---The ``Parent'' of Low Bowel Obstruction. Medicina (B Aires)2023: 875
12. States U. Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). Provisional Mortality Statistics by Multiple Cause of Death and by Single Race, for 2018 through Present2021:
13. Organization WH. International Statistical Classification of Diseases and Related Health Problems 10th Revision: World Health Organization; 2019 2019.
14. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008: 344
15. Ingram DD, Franco SJ. NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat. 2013: 1
16. Bureau USC. internet. 2025 [cited 2025 Sep 1]: Census Regions and Divisions of the United States.
17. Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998: 1
18. Program SR, Institute NC. Joinpoint Regression Software, Version 5.4.0 - April 2025. Bethesda, MD, USA: National Cancer Institute; 2025 [cited 2025 Sep 1]:
19. Lin Z, Zheng L, Chen Q, Guo Y, Zhao R, Xiao Y, Others. Nomogram for prediction of prolonged postoperative ileus after colorectal resection. BMC Cancer. 2022: 1017 https://doi.org/10.1186/s12885-022-10377-x]
20. Sueta T, Uchino M, Sasaki H, Koike Y, Takesue Y. Incidence and risk factors for prolonged postoperative ileus after laparoscopic surgery for colorectal cancer in older patients. BMC Surg. 2022: 69 https://doi.org/10.1186/s12893-022-01548-9]
21. Juo YY, Hyder O, Haider AH, Camp M, Lidor AO, Ahuja N. Ileus after colectomy in the modern era: a population-based analysis. Surgery. 2014: 1153 https://doi.org/10.1016/j.surg.2014.06.006]
22. Choi J, Kang J, Oh HK, Ahn S, Sohn DK, Kim DY, Others. Intraoperative hypothermia does not affect postoperative ileus after laparoscopic colorectal surgery. World J Surg. 2018: 1532 https://doi.org/10.1007/s00268-018-4515-5]
23. Hinoi T, Kawaguchi Y, Hattori M, Suzuki Y, Ohdan H. Postoperative ileus in an enhanced recovery pathway: retrospective cohort study. Int J Colorectal Dis. 2017: 411 https://doi.org/10.1007/s00384-016-2673-8]
24. Watanabe T, Miyake H, Morii K, Shiozawa M, Takeyama H. Predictive factors for postoperative ileus after elective right hemicolectomy with high ERAS compliance. Int J Colorectal Dis. 2024: 21 https://doi.org/10.1007/s00384-023-04400-2]
25. Boeding JRE, Ramphal W, Crolla RMPH, Boonman-de Winter LJM, Gobardhan PD, Schreinemakers JMJ. Ileus caused by obstructing colorectal cancer-impact on long-term survival. International journal of colorectal disease. 2018: 1393 https://doi.org/10.1007/s00384-018-3132-5]

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Waheed Qaisi, Mirna Hussein, Pakeezah Tabasum, Mohamed Wagdy, Nidal Mutawodeh, Abdallah Abdallah , Mohammed Mereb, Youssef Heikal