Abstract
Introduction: Managing idiopathic intracranial hypertension (IIH) is challenging due to limited treatment options. This study evaluates metformin as a potential therapy for IIH, examining its impact on disease outcomes and safety.
Methods: We performed a retrospective cohort study using the TriNetX database, covering data from 2009 to August 2024. The study included IIH patients, excluding those with other causes of raised intracranial pressure or pre-existing diabetes. Propensity score matching adjusted for age, sex, race, ethnicity, Hemoglobin A1C, and baseline BMI at metformin initiation. We assessed outcomes up to 24 months.
Results: Initially, 1,268 patients received metformin and 49,262 served as controls, showing disparities in various parameters. After matching, both groups consisted of 1,267 patients each. Metformin users had significantly lower risks of papilledema, headache, and refractory IIH at all follow-ups (p<0.0001). They also had fewer spinal punctures and reduced acetazolamide use. BMI reductions were more significant in the metformin group from 6 months onward (p<0.0001), with benefits persisting regardless of BMI changes. Metformin’s safety profile was comparable to the control group.
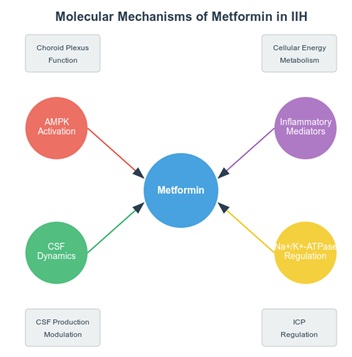
Conclusions: The study indicates metformin’s potential as a disease-modifying treatment in IIH, with improvements across multiple outcomes independent of weight loss. This suggests complex mechanisms at play, supporting further research through prospective clinical trials to confirm metformin’s role in IIH management and its mechanisms of action.
References
1. Mollan SP, Davies B, Silver NC, Shaw S, Mallucci CL, Wakerley BR, Krishnan A, Chavda SV, Ramalingam S, Edwards JJJoN, Neurosurgery, Psychiatry. Idiopathic intracranial hypertension: consensus guidelines on management2018: 1088
2. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013: 1159 [PMID: 23966248 10.1212/WNL.0b013e3182a55f17: 10.1212/WNL.0b013e3182a55f17]
3. Sinclair AJ, Burdon MA, Nightingale PG, Ball AK, Good P, Matthews TD, Jacks A, Lawden M, Clarke CE, Stewart PM, Walker EA, Tomlinson JW, Rauz S. Low energy diet and intracranial pressure in women with idiopathic intracranial hypertension: prospective cohort study. BMJ (Clinical research ed). 2010: c2701 [PMID: 20610512 10.1136/bmj.c2701: 10.1136/bmj.c2701]
4. Manfield JH, Yu KK, Efthimiou E, Darzi A, Athanasiou T, Ashrafian H. Bariatric Surgery or Non-surgical Weight Loss for Idiopathic Intracranial Hypertension? A Systematic Review and Comparison of Meta-analyses. Obesity surgery. 2017: 513 [PMID: 27981458 10.1007/s11695-016-2467-7: 10.1007/s11695-016-2467-7]
5. Ottridge R, Mollan SP, Botfield H, Frew E, Ives NJ, Matthews T, Mitchell J, Rick C, Singhal R, Woolley R, Sinclair AJ. Randomised controlled trial of bariatric surgery versus a community weight loss programme for the sustained treatment of idiopathic intracranial hypertension: the Idiopathic Intracranial Hypertension Weight Trial (IIH:WT) protocol. BMJ open. 2017: e017426 [PMID: 28963303 10.1136/bmjopen-2017-017426: 10.1136/bmjopen-2017-017426]
6. Wall M, McDermott MP, Kieburtz KD, Corbett JJ, Feldon SE, Friedman DI, Katz DM, Keltner JL, Schron EB, Kupersmith MJJJ. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial2014: 1641
7. Mollan SP, Aguiar M, Evison F, Frew E, Sinclair AJ. The expanding burden of idiopathic intracranial hypertension. Eye (London, England). 2019: 478 [PMID: 30356129 10.1038/s41433-018-0238-5: 10.1038/s41433-018-0238-5]
8. Mulla Y, Markey KA, Woolley RL, Patel S, Mollan SP, Sinclair AJ. Headache determines quality of life in idiopathic intracranial hypertension. The journal of headache and pain. 2015: 521 [PMID: 25982204 10.1186/s10194-015-0521-9: 10.1186/s10194-015-0521-9]
9. Schmickl CN, Owens RL, Orr JE, Edwards BA, Malhotra A. Side effects of acetazolamide: a systematic review and meta-analysis assessing overall risk and dose dependence. BMJ open respiratory research. 2020: [PMID: 32332024 10.1136/bmjresp-2020-000557: 10.1136/bmjresp-2020-000557]
10. Yri HM, Wegener M, Sander B, Jensen R. Idiopathic intracranial hypertension is not benign: a long-term outcome study. Journal of neurology. 2012: 886 [PMID: 22008872 10.1007/s00415-011-6273-9: 10.1007/s00415-011-6273-9]
11. Hornby C, Mollan SP, Botfield H, OʼReilly MW, Sinclair AJ. Metabolic Concepts in Idiopathic Intracranial Hypertension and Their Potential for Therapeutic Intervention. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2018: 522 [PMID: 29985799 10.1097/wno.0000000000000684: 10.1097/wno.0000000000000684]
12. Viollet B, Guigas B, Sanz Garcia N, Leclerc J, Foretz M, Andreelli F. Cellular and molecular mechanisms of metformin: an overview. Clinical science (London, England : 1979). 2012: 253 [PMID: 22117616 10.1042/cs20110386: 10.1042/cs20110386]
13. Botfield HF, Uldall MS, Westgate CSJ, Mitchell JL, Hagen SM, Gonzalez AM, Hodson DJ, Jensen RH, Sinclair AJ. A glucagon-like peptide-1 receptor agonist reduces intracranial pressure in a rat model of hydrocephalus. Science translational medicine. 2017: [PMID: 28835515 10.1126/scitranslmed.aan0972: 10.1126/scitranslmed.aan0972]
14. Karimy JK, Reeves BC, Damisah E, Duy PQ, Antwi P, David W, Wang K, Schiff SJ, Limbrick DD, Jr., Alper SL, Warf BC, Nedergaard M, Simard JM, Kahle KT. Inflammation in acquired hydrocephalus: pathogenic mechanisms and therapeutic targets. Nature reviews Neurology. 2020: 285 [PMID: 32152460 10.1038/s41582-020-0321-y: 10.1038/s41582-020-0321-y]
15. Łabuzek K, Suchy D, Gabryel B, Bielecka A, Liber S, Okopień B. Quantification of metformin by the HPLC method in brain regions, cerebrospinal fluid and plasma of rats treated with lipopolysaccharide. Pharmacological reports : PR. 2010: 956 [PMID: 21098880 10.1016/s1734-1140(10)70357-1: 10.1016/s1734-1140(10)70357-1]
16. Lin Z, Sun L. Research advances in treating metabolic syndrome. Frontiers in pharmacology. 2024: 1364881 [PMID: 39139641 10.3389/fphar.2024.1364881: 10.3389/fphar.2024.1364881]
17. Wardman JH, Andreassen SN, Toft-Bertelsen TL, Jensen MN, Wilhjelm JE, Styrishave B, Hamann S, Heegaard S, Sinclair AJ, MacAulay N. CSF hyperdynamics in rats mimicking the obesity and androgen excess characteristic of patients with idiopathic intracranial hypertension. Fluids and barriers of the CNS. 2024: 10 [PMID: 38273331 10.1186/s12987-024-00511-1: 10.1186/s12987-024-00511-1]
18. Palchuk MB, London JW, Perez-Rey D, Drebert ZJ, Winer-Jones JP, Thompson CN, Esposito J, Claerhout B. A global federated real-world data and analytics platform for research. JAMIA open. 2023: ooad035 [PMID: 37193038 10.1093/jamiaopen/ooad035: 10.1093/jamiaopen/ooad035]
19. Sun L, Xie C, Wang G, Wu Y, Wu Q, Wang X, Liu J, Deng Y, Xia J, Chen B, Zhang S, Yun C, Lian G, Zhang X, Zhang H, Bisson WH, Shi J, Gao X, Ge P, Liu C, Krausz KW, Nichols RG, Cai J, Rimal B, Patterson AD, Wang X, Gonzalez FJ, Jiang C. Gut microbiota and intestinal FXR mediate the clinical benefits of metformin. Nature medicine. 2018: 1919 [PMID: 30397356 10.1038/s41591-018-0222-4: 10.1038/s41591-018-0222-4]
20. Hornby C, Mollan SP, Mitchell J, Markey KA, Yangou A, Wright BLC, O'Reilly MW, Sinclair AJ. What Do Transgender Patients Teach Us About Idiopathic Intracranial Hypertension? Neuro-ophthalmology (Aeolus Press). 2017: 326 [PMID: 29238388 10.1080/01658107.2017.1316744: 10.1080/01658107.2017.1316744]
21. O'Reilly MW, Westgate CS, Hornby C, Botfield H, Taylor AE, Markey K, Mitchell JL, Scotton WJ, Mollan SP, Yiangou A, Jenkinson C, Gilligan LC, Sherlock M, Gibney J, Tomlinson JW, Lavery GG, Hodson DJ, Arlt W, Sinclair AJ. A unique androgen excess signature in idiopathic intracranial hypertension is linked to cerebrospinal fluid dynamics. JCI insight. 2019: [PMID: 30753168 10.1172/jci.insight.125348: 10.1172/jci.insight.125348]
22. Lashen H. Role of metformin in the management of polycystic ovary syndrome. Therapeutic advances in endocrinology and metabolism. 2010: 117 [PMID: 23148156 10.1177/2042018810380215: 10.1177/2042018810380215]
23. Lv WS, Wen JP, Li L, Sun RX, Wang J, Xian YX, Cao CX, Wang YL, Gao YY. The effect of metformin on food intake and its potential role in hypothalamic regulation in obese diabetic rats. Brain research. 2012: 11 [PMID: 22325091 10.1016/j.brainres.2012.01.028: 10.1016/j.brainres.2012.01.028]
24. DeFronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: Current perspectives on causes and risk. Metabolism: clinical and experimental. 2016: 20 [PMID: 26773926 10.1016/j.metabol.2015.10.014: 10.1016/j.metabol.2015.10.014
1. Mollan SP, Davies B, Silver NC, Shaw S, Mallucci CL, Wakerley BR, Krishnan A, Chavda SV, Ramalingam S, Edwards J, Hemmings K, Williamson M, Burdon MA, Hassan-Smith G, Digre K, Liu GT, Jensen RH, Sinclair AJ. Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol Neurosurg Psychiatry. 2018: 1088 [PMID: 29903905, https://doi.org/10.1136/jnnp-2017-317440]
2. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013: 1159 [PMID: 23966248, https://doi.org/10.1212/WNL.0b013e3182a55f17]
3. Sinclair AJ, Burdon MA, Nightingale PG, Ball AK, Good P, Matthews TD, Jacks A, Lawden M, Clarke CE, Stewart PM, Walker EA, Tomlinson JW, Rauz S. Low energy diet and intracranial pressure in women with idiopathic intracranial hypertension: prospective cohort study. BMJ (Clinical research ed). 2010: c2701 [PMID: 20610512, https://doi.org/10.1136/bmj.c2701]
4. Manfield JH, Yu KK, Efthimiou E, Darzi A, Athanasiou T, Ashrafian H. Bariatric Surgery or Non-surgical Weight Loss for Idiopathic Intracranial Hypertension? A Systematic Review and Comparison of Meta-analyses. Obesity surgery. 2017: 513 [PMID: 27981458, https://doi.org/10.1007/s11695-016-2467-7]
5. Ottridge R, Mollan SP, Botfield H, Frew E, Ives NJ, Matthews T, Mitchell J, Rick C, Singhal R, Woolley R, Sinclair AJ. Randomised controlled trial of bariatric surgery versus a community weight loss programme for the sustained treatment of idiopathic intracranial hypertension: the Idiopathic Intracranial Hypertension Weight Trial (IIH:WT) protocol. BMJ open. 2017: e017426 [PMID: 28963303, https://doi.org/10.1136/bmjopen-2017-017426]
6. Committee NIIHSGW, Wall M, McDermott MP, Kieburtz KD, Corbett JJ, Feldon SE, Friedman DI, Katz DM, Keltner JL, Schron EB, Kupersmith MJ. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA. 2014: 1641 [PMID: 24756514, https://doi.org/10.1001/jama.2014.3312]
7. Mollan SP, Aguiar M, Evison F, Frew E, Sinclair AJ. The expanding burden of idiopathic intracranial hypertension. Eye (London, England). 2019: 478 [PMID: 30356129, https://doi.org/10.1038/s41433-018-0238-5]
8. Mulla Y, Markey KA, Woolley RL, Patel S, Mollan SP, Sinclair AJ. Headache determines quality of life in idiopathic intracranial hypertension. The journal of headache and pain. 2015: 521 [PMID: 25982204, https://doi.org/10.1186/s10194-015-0521-9]
9. Schmickl CN, Owens RL, Orr JE, Edwards BA, Malhotra A. Side effects of acetazolamide: a systematic review and meta-analysis assessing overall risk and dose dependence. BMJ open respiratory research. 2020: [PMID: 32332024, https://doi.org/10.1136/bmjresp-2020-000557]
10. Yri HM, Wegener M, Sander B, Jensen R. Idiopathic intracranial hypertension is not benign: a long-term outcome study. Journal of neurology. 2012: 886 [PMID: 22008872, https://doi.org/10.1007/s00415-011-6273-9]
11. Hornby C, Mollan SP, Botfield H, O'Reilly MW, Sinclair AJ. Metabolic Concepts in Idiopathic Intracranial Hypertension and Their Potential for Therapeutic Intervention. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2018: 522 [PMID: 29985799, https://doi.org/10.1097/WNO.0000000000000684]
12. Viollet B, Guigas B, Sanz Garcia N, Leclerc J, Foretz M, Andreelli F. Cellular and molecular mechanisms of metformin: an overview. Clinical science (London, England : 1979). 2012: 253 [PMID: 22117616, https://doi.org/10.1042/CS20110386]
13. Botfield HF, Uldall MS, Westgate CSJ, Mitchell JL, Hagen SM, Gonzalez AM, Hodson DJ, Jensen RH, Sinclair AJ. A glucagon-like peptide-1 receptor agonist reduces intracranial pressure in a rat model of hydrocephalus. Science translational medicine. 2017: [PMID: 28835515, https://doi.org/10.1126/scitranslmed.aan0972]
14. Karimy JK, Reeves BC, Damisah E, Duy PQ, Antwi P, David W, Wang K, Schiff SJ, Limbrick DD, Jr., Alper SL, Warf BC, Nedergaard M, Simard JM, Kahle KT. Inflammation in acquired hydrocephalus: pathogenic mechanisms and therapeutic targets. Nature reviews Neurology. 2020: 285 [PMID: 32152460, https://doi.org/10.1038/s41582-020-0321-y]
15. Labuzek K, Suchy D, Gabryel B, Bielecka A, Liber S, Okopien B. Quantification of metformin by the HPLC method in brain regions, cerebrospinal fluid and plasma of rats treated with lipopolysaccharide. Pharmacological reports : PR. 2010: 956 [PMID: 21098880, https://doi.org/10.1016/s1734-1140(10)70357-1]
16. Lin Z, Sun L. Research advances in the therapy of metabolic syndrome. Frontiers in pharmacology. 2024: 1364881 [PMID: 39139641, https://doi.org/10.3389/fphar.2024.1364881]
17. Wardman JH, Andreassen SN, Toft-Bertelsen TL, Jensen MN, Wilhjelm JE, Styrishave B, Hamann S, Heegaard S, Sinclair AJ, MacAulay N. CSF hyperdynamics in rats mimicking the obesity and androgen excess characteristic of patients with idiopathic intracranial hypertension. Fluids and barriers of the CNS. 2024: 10 [PMID: 38273331, https://doi.org/10.1186/s12987-024-00511-1]
18. Palchuk MB, London JW, Perez-Rey D, Drebert ZJ, Winer-Jones JP, Thompson CN, Esposito J, Claerhout B. A global federated real-world data and analytics platform for research. JAMIA open. 2023: ooad035 [PMID: 37193038, https://doi.org/10.1093/jamiaopen/ooad035]
19. Sun L, Xie C, Wang G, Wu Y, Wu Q, Wang X, Liu J, Deng Y, Xia J, Chen B, Zhang S, Yun C, Lian G, Zhang X, Zhang H, Bisson WH, Shi J, Gao X, Ge P, Liu C, Krausz KW, Nichols RG, Cai J, Rimal B, Patterson AD, Wang X, Gonzalez FJ, Jiang C. Gut microbiota and intestinal FXR mediate the clinical benefits of metformin. Nature medicine. 2018: 1919 [PMID: 30397356, https://doi.org/10.1038/s41591-018-0222-4]
20. Hornby C, Mollan SP, Mitchell J, Markey KA, Yangou A, Wright BLC, O'Reilly MW, Sinclair AJ. What Do Transgender Patients Teach Us About Idiopathic Intracranial Hypertension? Neuro-ophthalmology (Aeolus Press). 2017: 326 [PMID: 29238388, https://doi.org/10.1080/01658107.2017.1316744]
21. O'Reilly MW, Westgate CS, Hornby C, Botfield H, Taylor AE, Markey K, Mitchell JL, Scotton WJ, Mollan SP, Yiangou A, Jenkinson C, Gilligan LC, Sherlock M, Gibney J, Tomlinson JW, Lavery GG, Hodson DJ, Arlt W, Sinclair AJ. A unique androgen excess signature in idiopathic intracranial hypertension is linked to cerebrospinal fluid dynamics. JCI insight. 2019: [PMID: 30753168, https://doi.org/10.1172/jci.insight.125348]
22. Lashen H. Role of metformin in the management of polycystic ovary syndrome. Therapeutic advances in endocrinology and metabolism. 2010: 117 [PMID: 23148156, https://doi.org/10.1177/2042018810380215]
23. Lv WS, Wen JP, Li L, Sun RX, Wang J, Xian YX, Cao CX, Wang YL, Gao YY. The effect of metformin on food intake and its potential role in hypothalamic regulation in obese diabetic rats. Brain research. 2012: 11 [PMID: 22325091, https://doi.org/10.1016/j.brainres.2012.01.028]
24. DeFronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: Current perspectives on causes and risk. Metabolism: clinical and experimental. 2016: 20 [PMID: 26773926, https://doi.org/10.1016/j.metabol.2015.10.014]

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2024 Ahmed Y. Azzam, Mahmoud Nassar, Ahmed Saad Al Zomia, Adam Elswedy, Mahmoud M. Morsy, Adham A. Mohamed, Osman Elamin, Omar S. Elsayed, Mohammed A. Azab, Muhammed Amir Essibayi, Jin Wu, Adam A. Dmytirw, David J. Altschul