Abstract
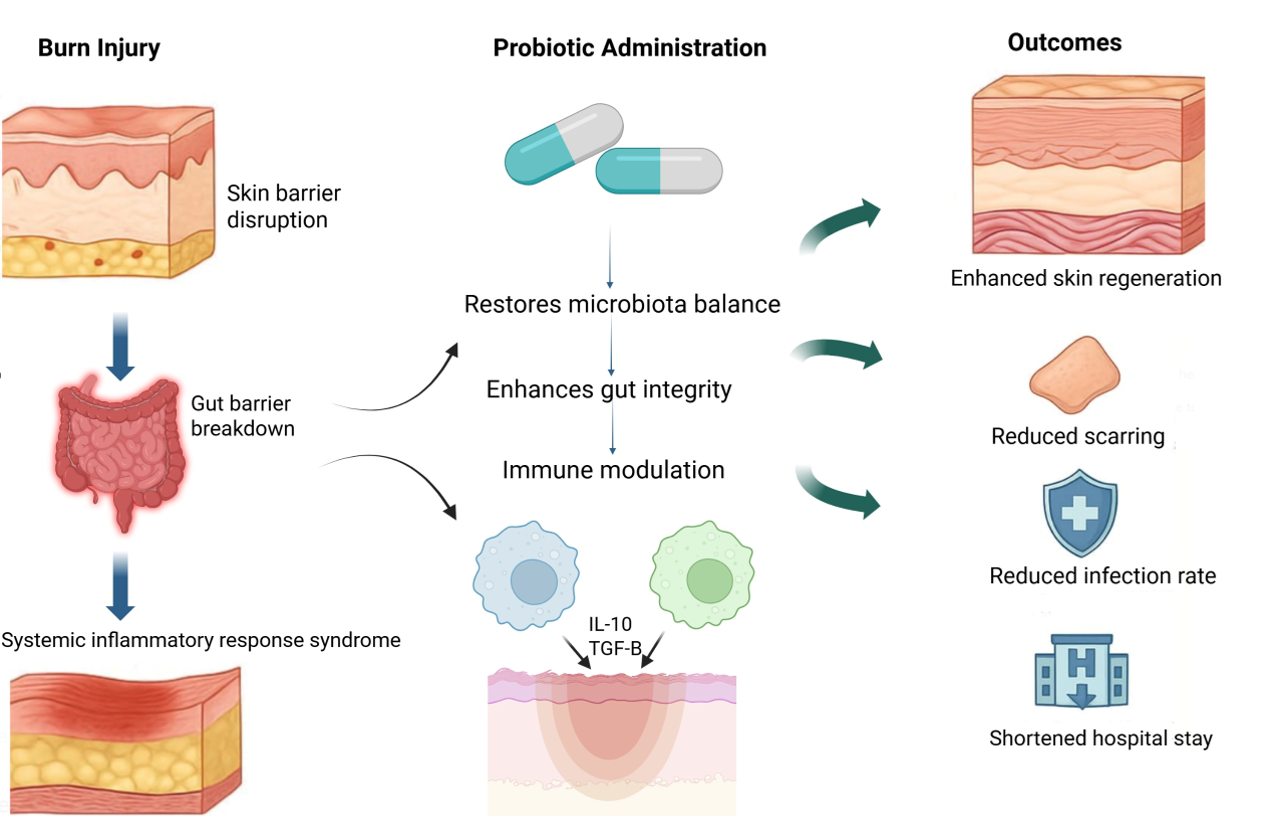
This review explores the potential therapeutic benefits of probiotics in the treatment of burn injuries, with the aim of addressing the limitations of traditional therapeutic approaches. It offers a comprehensive analysis of burn pathophysiology, including a wide range of burn forms and the biological reactions they induce, such as pain, inflammation, fluid imbalance, and metabolic alterations. It also specifically explains the mechanisms by which probiotics contribute to the improved healing of wounds and modified gut microbiota, as they are particularly effective in these two directions. This study looks at the ways probiotic treatment can facilitate the regeneration of the skin, which is crucial for accelerating burn recovery . Furthermore, it examines the barriers and limits of probiotic therapy, such as strain regularity and safety issues in immunocompromised patients, while emphasizing the interdependent benefits of probiotics and nutrition in promoting burn healing. This review highlights the advantages of probiotics in burn management and their potential as an adjuvant therapy for enhancing treatment results and patient well-being in the burn care context.
References
1. Sanchez B, Delgado S, Blanco-Miguez A, Lourenco A, Gueimonde M, Margolles A. Probiotics, gut microbiota, and their influence on host health and disease. Mol Nutr Food Res. 2017: [PMID: 27500859, https://doi.org/10.1002/mnfr.201600240]
2. Iddins CJ, DiCarlo AL, Ervin MD, Herrera-Reyes E, Goans RE. Cutaneous and local radiation injuries. J Radiol Prot. 2022: [PMID: 34488201, https://doi.org/10.1088/1361-6498/ac241a]
3. Delano MJ, Ward PA. The immune system's role in sepsis progression, resolution, and long-term outcome. Immunol Rev. 2016: 330 [PMID: 27782333, https://doi.org/10.1111/imr.12499]
4. Corcione S, Lupia T, De Rosa FG, Host, Microbiota Interaction Study Group of the European Society of Clinical M, Infectious D. Microbiome in the setting of burn patients: implications for infections and clinical outcomes. Burns Trauma. 2020: tkaa033 [PMID: 32821744, https://doi.org/10.1093/burnst/tkaa033]
5. Weinand C. Associated bacterial and fungal infections in burn wounds: Common factors, distribution in etiology, age groups, bacterial and fungal strands – Evaluation of a single burn center experience of 20 years. Burns Open. 2024: https://doi.org/10.1016/j.burnso.2024.100363]
6. Kaistha SD, Deshpande N. Traditional Probiotics, Next-Generation Probiotics, and Engineered Live Biotherapeutic Products in Chronic Wound Healing. Springer. 247 https://doi.org/10.1007/978-981-16-2677-7_8]
7. El-Ghazely MH, Mahmoud WH, Atia MA, Eldip EM. Effect of probiotic administration in the therapy of pediatric thermal burn. Ann Burns Fire Disasters. 2016: 268 [PMID: 28289360,
8. Notay M, Saric-Bosanac S, Vaughn AR, Dhaliwal S, Trivedi M, Reiter PN, Rybak I, Li CC, Weiss LB, Ambrogio L, Burney W, Sivamani RK. The use of topical Nitrosomonas eutropha for cosmetic improvement of facial wrinkles. J Cosmet Dermatol. 2020: 689 [PMID: 31257694, https://doi.org/10.1111/jocd.13060]
9. Jung YO, Jeong H, Cho Y, Lee EO, Jang HW, Kim J, Nam K, Lim KM. Lysates of a Probiotic, Lactobacillus rhamnosus, Can Improve Skin Barrier Function in a Reconstructed Human Epidermis Model. Int J Mol Sci. 2019: [PMID: 31480681, https://doi.org/10.3390/ijms20174289]
10. Im AR, Lee B, Kang DJ, Chae S. Protective effects of tyndallized Lactobacillus acidophilus IDCC 3302 against UVB‑induced photodamage to epidermal keratinocytes cells. Int J Mol Med. 2019: 2499 [PMID: 31017257, https://doi.org/10.3892/ijmm.2019.4161]
11. Knackstedt R, Knackstedt T, Gatherwright J. The role of topical probiotics on wound healing: A review of animal and human studies. Int Wound J. 2020: 1687 [PMID: 32869480, https://doi.org/10.1111/iwj.13451]
12. Oryan A, Jalili M, Kamali A, Nikahval B. The concurrent use of probiotic microorganism and collagen hydrogel/scaffold enhances burn wound healing: An in vivo evaluation. Burns. 2018: 1775 [PMID: 30078473, https://doi.org/10.1016/j.burns.2018.05.016]
13. Capurso L. Thirty Years of Lactobacillus rhamnosus GG: A Review. J Clin Gastroenterol. 2019: S1 [PMID: 30741841, https://doi.org/10.1097/MCG.0000000000001170]
14. Rocchetti MT, Russo P, Capozzi V, Drider D, Spano G, Fiocco D. Bioprospecting Antimicrobials from Lactiplantibacillus plantarum: Key Factors Underlying Its Probiotic Action. Int J Mol Sci. 2021: [PMID: 34769500, https://doi.org/10.3390/ijms222112076]
15. Gilliam CH, Brazelton de Cardenas J, Carias D, Maron Alfaro G, Hayden RT, Hakim H. Lactobacillus bloodstream infections genetically related to probiotic use in pediatric hematopoietic cell transplant patients. Infect Control Hosp Epidemiol. 2023: 484 [PMID: 35225182, https://doi.org/10.1017/ice.2021.515]
16. Eze UJ, Lal A, Elkoush MI, Halytska M, Atif S. Recurrent Lactobacillus Rhamnoses Bacteremia and Complications in an Immunocompromised Patient With History of Probiotic Use: A Case Report. Cureus. 2024: e54879 [PMID: 38550408, https://doi.org/10.7759/cureus.54879]
17. Haranahalli Nataraj B, Behare PV, Yadav H, Srivastava AK. Emerging pre-clinical safety assessments for potential probiotic strains: a review. Crit Rev Food Sci Nutr. 2024: 8155 [PMID: 37039078, https://doi.org/10.1080/10408398.2023.2197066]
18. Soleymanzadeh Moghadam S, Momeni M, Mazar Atabaki S, Mousavi Shabestari T, Boustanshenas M, Afshar M, Roham M. Topical Treatment of Second-Degree Burn Wounds with Lactobacillus plantarum Supernatant: Phase I Trial. Iran J Pathol. 2022: 460 [PMID: 36532643, https://doi.org/10.30699/ijp.2022.551202.2863]
19. Almadani YH, Vorstenbosch J, Davison PG, Murphy AM. Wound Healing: A Comprehensive Review. Semin Plast Surg. 2021: 141 [PMID: 34526860, https://doi.org/10.1055/s-0041-1731791]
20. Castana O, Anagiotos G, Rempelos G, Adalopoulou A, Kokkinakis C, Giannakidou M, Diplas DB, Alexakis D. Pain response and pain control in burn patients. Ann Burns Fire Disasters. 2009: 88 [PMID: 21991161,
21. Clark A, Imran J, Madni T, Wolf SE. Nutrition and metabolism in burn patients. Burns Trauma. 2017: 11 [PMID: 28428966, https://doi.org/10.1186/s41038-017-0076-x]
22. Markiewicz-Gospodarek A, Koziol M, Tobiasz M, Baj J, Radzikowska-Buchner E, Przekora A. Burn Wound Healing: Clinical Complications, Medical Care, Treatment, and Dressing Types: The Current State of Knowledge for Clinical Practice. Int J Environ Res Public Health. 2022: [PMID: 35162360, https://doi.org/10.3390/ijerph19031338]
23. Luck ME, Herrnreiter CJ, Choudhry MA. Gut Microbial Changes and their Contribution to Post-Burn Pathology. Shock. 2021: 329 [PMID: 33481548, https://doi.org/10.1097/SHK.0000000000001736]
24. Shimizu K, Ogura H, Asahara T, Nomoto K, Matsushima A, Hayakawa K, Ikegawa H, Tasaki O, Kuwagata Y, Shimazu T. Gut microbiota and environment in patients with major burns - a preliminary report. Burns. 2015: e28 [PMID: 25465986, https://doi.org/10.1016/j.burns.2014.10.019]
25. McMahan RH, Boe DM, Walrath TM, Idrovo JP, Kovacs EJ. Aging, Cutaneous Burn Injury and Multi-Organ Complications: The Role of the Gut. Adv Geriatr Med Res. 2022: [PMID: 35913894, https://doi.org/10.20900/agmr20220004]
26. Pan YY, Fan YF, Li JL, Cui SY, Huang N, Jin GY, Chen C, Zhang C. [Analysis of the dynamic changes in gut microbiota in patients with extremely severe burns by 16S ribosomal RNA high-throughput sequencing technology]. Zhonghua Shao Shang Za Zhi. 2020: 1159 [PMID: 33379852, https://doi.org/10.3760/cma.j.cn501120-20200518-00271]
27. Lima KM, Davis RR, Liu SY, Greenhalgh DG, Tran NK. Longitudinal profiling of the burn patient cutaneous and gastrointestinal microbiota: a pilot study. Sci Rep. 2021: 10667 [PMID: 34021204, https://doi.org/10.1038/s41598-021-89822-z]
28. Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar Reddy D. Role of the normal gut microbiota. World J Gastroenterol. 2015: 8787 [PMID: 26269668, https://doi.org/10.3748/wjg.v21.i29.8787]
29. Rooks MG, Garrett WS. Gut microbiota, metabolites and host immunity. Nat Rev Immunol. 2016: 341 [PMID: 27231050, https://doi.org/10.1038/nri.2016.42]
30. Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nat Rev Dis Primers. 2020: 11 [PMID: 32054846, https://doi.org/10.1038/s41572-020-0145-5]
31. Earley ZM, Akhtar S, Green SJ, Naqib A, Khan O, Cannon AR, Hammer AM, Morris NL, Li X, Eberhardt JM, Gamelli RL, Kennedy RH, Choudhry MA. Burn Injury Alters the Intestinal Microbiome and Increases Gut Permeability and Bacterial Translocation. PLoS One. 2015: e0129996 [PMID: 26154283, https://doi.org/10.1371/journal.pone.0129996]
32. Wrba L, Palmer A, Braun CK, Huber-Lang M. Evaluation of gut-blood barrier dysfunction in various models of trauma, hemorrhagic shock, and burn injury. J Trauma Acute Care Surg. 2017: 944 [PMID: 28700414, https://doi.org/10.1097/TA.0000000000001654]
33. Odamaki T, Kato K, Sugahara H, Hashikura N, Takahashi S, Xiao JZ, Abe F, Osawa R. Age-related changes in gut microbiota composition from newborn to centenarian: a cross-sectional study. BMC Microbiol. 2016: 90 [PMID: 27220822, https://doi.org/10.1186/s12866-016-0708-5]
34. Zhang CX, Wang HY, Chen TX. Interactions between Intestinal Microflora/Probiotics and the Immune System. Biomed Res Int. 2019: 6764919 [PMID: 31828119, https://doi.org/10.1155/2019/6764919]
35. Wang X, Zhang P, Zhang X. Probiotics Regulate Gut Microbiota: An Effective Method to Improve Immunity. Molecules. 2021: [PMID: 34641619, https://doi.org/10.3390/molecules26196076]
36. Stavrou G, Kotzampassi K. Gut microbiome, surgical complications and probiotics. Ann Gastroenterol. 2017: 45 [PMID: 28042237, https://doi.org/10.20524/aog.2016.0086]
37. Maldonado Galdeano C, Cazorla SI, Lemme Dumit JM, Velez E, Perdigon G. Beneficial Effects of Probiotic Consumption on the Immune System. Ann Nutr Metab. 2019: 115 [PMID: 30673668, https://doi.org/10.1159/000496426]
38. La Fata G, Weber P, Mohajeri MH. Probiotics and the Gut Immune System: Indirect Regulation. Probiotics Antimicrob Proteins. 2018: 11 [PMID: 28861741, https://doi.org/10.1007/s12602-017-9322-6]
39. Liu Q, Yu Z, Tian F, Zhao J, Zhang H, Zhai Q, Chen W. Surface components and metabolites of probiotics for regulation of intestinal epithelial barrier. Microb Cell Fact. 2020: 23 [PMID: 32024520, https://doi.org/10.1186/s12934-020-1289-4]
40. Rocha-Ramirez LM, Perez-Solano RA, Castanon-Alonso SL, Moreno Guerrero SS, Ramirez Pacheco A, Garcia Garibay M, Eslava C. Probiotic Lactobacillus Strains Stimulate the Inflammatory Response and Activate Human Macrophages. J Immunol Res. 2017: 4607491 [PMID: 28758133, https://doi.org/10.1155/2017/4607491]
41. Grice EA, Segre JA. The skin microbiome. Nat Rev Microbiol. 2011: 244 [PMID: 21407241, https://doi.org/10.1038/nrmicro2537]
42. Stecker RA, Moon JM, Russo TJ, Ratliff KM, Mumford PW, Jager R, Purpura M, Kerksick CM. Bacillus coagulans GBI-30, 6086 improves amino acid absorption from milk protein. Nutr Metab (Lond). 2020: 93 [PMID: 33110439, https://doi.org/10.1186/s12986-020-00515-2]
43. Canchy L, Kerob D, Demessant A, Amici JM. Wound healing and microbiome, an unexpected relationship. J Eur Acad Dermatol Venereol. 2023: 7 [PMID: 36635613, https://doi.org/10.1111/jdv.18854]
44. Bates M. The Role of the Skin Microbiome in Health and Disease. IEEE Pulse. 2022: 8 [PMID: 36044472, https://doi.org/10.1109/MPULS.2022.3191384]
45. Mahmud MR, Akter S, Tamanna SK, Mazumder L, Esti IZ, Banerjee S, Akter S, Hasan MR, Acharjee M, Hossain MS, Pirttila AM. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022: 2096995 [PMID: 35866234, https://doi.org/10.1080/19490976.2022.2096995]
46. Habeebuddin M, Karnati RK, Shiroorkar PN, Nagaraja S, Asdaq SMB, Khalid Anwer M, Fattepur S. Topical Probiotics: More Than a Skin Deep. Pharmaceutics. 2022: [PMID: 35335933, https://doi.org/10.3390/pharmaceutics14030557]
47. Sharma G, Khanna G, Sharma P, Deol PK, Kaur IP. Mechanistic Role of Probiotics in Improving Skin Health. In: Beri K, Deol PK, Sandhu SK, editors. Probiotic Research in Therapeutics2022. p. 27-47.
48. Lukic J, Chen V, Strahinic I, Begovic J, Lev-Tov H, Davis SC, Tomic-Canic M, Pastar I. Probiotics or pro-healers: the role of beneficial bacteria in tissue repair. Wound Repair Regen. 2017: 912 [PMID: 29315980, https://doi.org/10.1111/wrr.12607]
49. Horseman TS, Frank AM, Shupp JW, Burmeister DM. Meta-Analysis of Publicly Available Clinical and Preclinical Microbiome Data From Studies of Burn Injury. J Burn Care Res. 2023: 1041 [PMID: 37352011, https://doi.org/10.1093/jbcr/irad098]
50. Maslova E, Osman S, McCarthy RR. Using the Galleria mellonella burn wound and infection model to identify and characterize potential wound probiotics. Microbiology (Reading). 2023: [PMID: 37350463, https://doi.org/10.1099/mic.0.001350]
51. Mayes T, Gottschlich MM, James LE, Allgeier C, Weitz J, Kagan RJ. Clinical safety and efficacy of probiotic administration following burn injury. J Burn Care Res. 2015: 92 [PMID: 25559730, https://doi.org/10.1097/BCR.0000000000000139]
52. Shrivastava S, Bhatu N. A Study on the Usage of Probiotics as a Safer Antipyretic. Journal of Cellular Signaling. 2023: 73 https://doi.org/10.33696/Signaling.4.093]
53. Bremmer F, Strobel P. [Mediastinal germ cell tumors]. Pathologe. 2016: 441 [PMID: 27491549, https://doi.org/10.1007/s00292-016-0196-2]
54. Wang X, Yang Y, Huycke MM. Risks associated with enterococci as probiotics. Food Res Int. 2020: 108788 [PMID: 32036912, https://doi.org/10.1016/j.foodres.2019.108788]
55. Golchin A, Ranjbarvan P, Parviz S, Shokati A, Naderi R, Rasmi Y, Kiani S, Moradi F, Heidari F, Saltanatpour Z, Alizadeh A. The role of probiotics in tissue engineering and regenerative medicine. Regen Med. 2023: 635 [PMID: 37492007, https://doi.org/10.2217/rme-2022-0209]
56. Han Y, Ren QL. Does probiotics work for bacterial vaginosis and vulvovaginal candidiasis. Curr Opin Pharmacol. 2021: 83 [PMID: 34649216, https://doi.org/10.1016/j.coph.2021.09.004]
57. Neveling DP, Dicks LMT. Probiotics: an Antibiotic Replacement Strategy for Healthy Broilers and Productive Rearing. Probiotics Antimicrob Proteins. 2021: 1 [PMID: 32556932, https://doi.org/10.1007/s12602-020-09640-z]
58. Peral MC, Martinez MA, Valdez JC. Bacteriotherapy with Lactobacillus plantarum in burns. Int Wound J. 2009: 73 [PMID: 19291120, https://doi.org/10.1111/j.1742-481X.2008.00577.x]
59. Thomson CH, Hassan I, Dunn K. Yakult: a role in combating multi-drug resistant Pseudomonas aeruginosa? J Wound Care. 2012: 566 [PMID: 23413495, https://doi.org/10.12968/jowc.2012.21.11.566]

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Kholoud Al Jebawi, Jobran Toami, Adel Ayash, Razan Salha, Mira Al Shoufy, Jamil Nasrallah , Naseeb Danaf, Lea El Ghawi, Layal Msheik, Hiba Hamdar