Abstract
Introduction: Diabetes mellitus represents a significant public health challenge, however, the current trends in its epidemiology remain incompletely characterized. This study aimed to analyze epidemiological changes and demographic patterns in diabetes incidence and prevalence across the United States from 1990 to 2024.
Methods: We conducted a retrospective cohort study utilizing the TriNetX Global Health Research Network, analyzing de-identified electronic health records from 52,922,301 patients across 92 U.S. healthcare organizations. Time-based changes in disease trends regarding diabetes incidence and prevalence were targeted, and stratified by age, sex, race, and diabetes type.
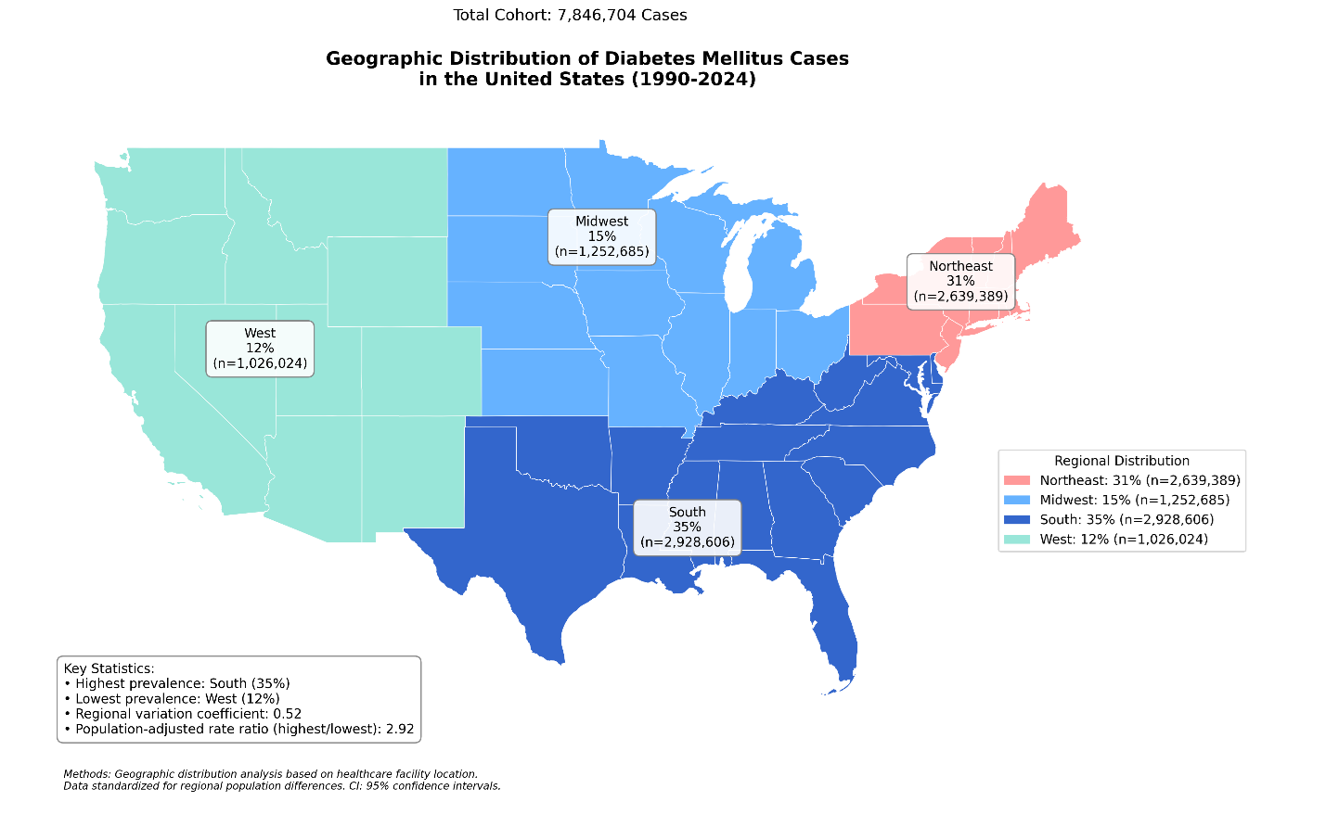
Results: Combined diabetes incidence increased from 3.98 per 1,000 in 1990-1994 to 60.98 per 1,000 in 2020-2024, while prevalence doubled from 6.26% to 12.00%. T2DM showed a twenty-fold increase in incidence (3.52 to 59.30 per 1,000), while T1DM peaked at 7.46 per 1,000 in 2010-2014 before declining to 4.59 per 1,000. Significant disparities were observed across demographic groups, with the highest rates among Native Hawaiians/Pacific Islanders (incidence: 94.75 per 1,000; prevalence: 20.65%) and consistent male predominance (incidence: 69.40 vs 54.07 per 1,000).
Conclusions: These findings reveal concerning trends in diabetes epidemiology, characterized by a prominent and significant elevation in disease burden and persistent demographic disparities. The results call for the urgent need for optimized preventive strategies, targeted interventions for high-risk populations, and systematic changes in healthcare delivery to address this growing public health challenge effectively.
References
1. Collaborators GBDD. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet (London, England). 2023: 203 [PMID: 37356446 https://doi.org/10.1016/S0140-6736(23)01301-6]
2. Xu Y, Yan M, Fu C, Xu W, Liu Y, Li Y. Complex patterns and determinants of regional multiple chronic conditions across the United States. PNAS nexus. 2024: pgae513 [PMID: 39660060 https://doi.org/10.1093/pnasnexus/pgae513]
3. Pilla SJ, Rooney MR, McCoy RG. Disability and Diabetes in Adults. In: Lawrence JM, Casagrande SS, Herman WH, Wexler DJ, Cefalu WT, editors. Diabetes in America. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); 2023.
4. Fang L, Sheng H, Tan Y, Zhang Q. Prevalence of diabetes in the USA from the perspective of demographic characteristics, physical indicators and living habits based on NHANES 2009-2018. Frontiers in endocrinology. 2023: 1088882 [PMID: 36960397 https://doi.org/10.3389/fendo.2023.1088882]
5. Fang M, Wang D, Coresh J, Selvin E. Undiagnosed Diabetes in U.S. Adults: Prevalence and Trends. Diabetes care. 2022: 1994 [PMID: 35817030 https://doi.org/10.2337/dc22-0242]
6. In: Cowie CC, Casagrande SS, Menke A, Cissell MA, Eberhardt MS, Meigs JB, Gregg EW, Knowler WC, Barrett-Connor E, Becker DJ, Brancati FL, Boyko EJ, Herman WH, Howard BV, Narayan KMV, Rewers M, Fradkin JE, editors. Diabetes in America. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (US); 2018.
7. Duan D, Kengne AP, Echouffo-Tcheugui JB. Screening for Diabetes and Prediabetes. Endocrinology and metabolism clinics of North America. 2021: 369 [PMID: 34399951 https://doi.org/10.1016/j.ecl.2021.05.002]
8. Hassan S, Gujral UP, Quarells RC, Rhodes EC, Shah MK, Obi J, Lee WH, Shamambo L, Weber MB, Narayan KMV. Disparities in diabetes prevalence and management by race and ethnicity in the USA: defining a path forward. The lancet Diabetes & endocrinology. 2023: 509 [PMID: 37356445 https://doi.org/10.1016/S2213-8587(23)00129-8]
9. Foss R, Fischer K, Lampman MA, Laabs S, Halasy M, Allen SV, Garrison GM, Sobolik G, Bernard M, Sosso J, Thacher TD. Disparities in Diabetes Care: Differences Between Rural and Urban Patients Within a Large Health System. Annals of family medicine. 2023: 234 [PMID: 37217319 https://doi.org/10.1370/afm.2962]
10. Mikhail N, Wali S, Brown AF. Ethnic Disparities in Diabetes. Endocrinology and metabolism clinics of North America. 2021: 475 [PMID: 34399957 https://doi.org/10.1016/j.ecl.2021.05.006]
11. Liu J, Yi SS, Russo R, Mayer VL, Wen M, Li Y. Trends and disparities in diabetes and prediabetes among adults in the United States, 1999-2018. Public health. 2023: 163 [PMID: 36586345 https://doi.org/10.1016/j.puhe.2022.10.021]
12. Palchuk MB, London JW, Perez-Rey D, Drebert ZJ, Winer-Jones JP, Thompson CN, Esposito J, Claerhout B. A global federated real-world data and analytics platform for research. JAMIA open. 2023: ooad035 [PMID: 37193038 https://doi.org/10.1093/jamiaopen/ooad035]
13. American Diabetes Association Professional Practice C. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes-2024. Diabetes care. 2024: S11 [PMID: 38078573 https://doi.org/10.2337/dc24-S001]
14. Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P, Expert Committee on the D, Classification of Diabetes M. Follow-up report on the diagnosis of diabetes mellitus. Diabetes care. 2003: 3160 [PMID: 14578255 https://doi.org/10.2337/diacare.26.11.3160]
15. American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes care. 2010: S62 [PMID: 20042775 https://doi.org/10.2337/dc10-S062]
16. Siu AL, Force USPST. Screening for Abnormal Blood Glucose and Type 2 Diabetes Mellitus: U.S. Preventive Services Task Force Recommendation Statement. Annals of internal medicine. 2015: 861 [PMID: 26501513 https://doi.org/10.7326/M15-2345]
17. American Diabetes A. Standards of medical care in diabetes--2014. Diabetes care. 2014: S14 [PMID: 24357209 https://doi.org/10.2337/dc14-S014]
18. Riddle MC, Cefalu WT, Evans PH, Gerstein HC, Nauck MA, Oh WK, Rothberg AE, le Roux CW, Rubino F, Schauer P, Taylor R, Twenefour D. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes care. 2021: 2438 [PMID: 34462270 https://doi.org/10.2337/dci21-0034]
19. Look ARG, Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, Coday M, Crow RS, Curtis JM, Egan CM, Espeland MA, Evans M, Foreyt JP, Ghazarian S, Gregg EW, Harrison B, Hazuda HP, Hill JO, Horton ES, Hubbard VS, Jakicic JM, Jeffery RW, Johnson KC, Kahn SE, Kitabchi AE, Knowler WC, Lewis CE, Maschak-Carey BJ, Montez MG, Murillo A, Nathan DM, Patricio J, Peters A, Pi-Sunyer X, Pownall H, Reboussin D, Regensteiner JG, Rickman AD, Ryan DH, Safford M, Wadden TA, Wagenknecht LE, West DS, Williamson DF, Yanovski SZ. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. The New England journal of medicine. 2013: 145 [PMID: 23796131 https://doi.org/10.1056/NEJMoa1212914]
20. Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, Lau ESH, Eliasson B, Kong APS, Ezzati M, Aguilar-Salinas CA, McGill M, Levitt NS, Ning G, So WY, Adams J, Bracco P, Forouhi NG, Gregory GA, Guo J, Hua X, Klatman EL, Magliano DJ, Ng BP, Ogilvie D, Panter J, Pavkov M, Shao H, Unwin N, White M, Wou C, Ma RCW, Schmidt MI, Ramachandran A, Seino Y, Bennett PH, Oldenburg B, Gagliardino JJ, Luk AOY, Clarke PM, Ogle GD, Davies MJ, Holman RR, Gregg EW. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet (London, England). 2021: 2019 [PMID: 33189186 https://doi.org/10.1016/S0140-6736(20)32374-6]
21. Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. The lancet Diabetes & endocrinology. 2014: 56 [PMID: 24622669 https://doi.org/10.1016/S2213-8587(13)70112-8]
22. Nordstrom A, Hadrevi J, Olsson T, Franks PW, Nordstrom P. Higher Prevalence of Type 2 Diabetes in Men Than in Women Is Associated With Differences in Visceral Fat Mass. The Journal of clinical endocrinology and metabolism. 2016: 3740 [PMID: 27490920 https://doi.org/10.1210/jc.2016-1915]
23. Peters SAE, Woodward M. Sex Differences in the Burden and Complications of Diabetes. Current diabetes reports. 2018: 33 [PMID: 29671082 https://doi.org/10.1007/s11892-018-1005-5]
24. Cheng YJ, Kanaya AM, Araneta MRG, Saydah SH, Kahn HS, Gregg EW, Fujimoto WY, Imperatore G. Prevalence of Diabetes by Race and Ethnicity in the United States, 2011-2016. Jama. 2019: 2389 [PMID: 31860047 https://doi.org/10.1001/jama.2019.19365]
25. Vehik K, Lynch KF, Wong MC, Tian X, Ross MC, Gibbs RA, Ajami NJ, Petrosino JF, Rewers M, Toppari J, Ziegler AG, She JX, Lernmark A, Akolkar B, Hagopian WA, Schatz DA, Krischer JP, Hyoty H, Lloyd RE, Group TS. Prospective virome analyses in young children at increased genetic risk for type 1 diabetes. Nature medicine. 2019: 1865 [PMID: 31792456 https://doi.org/10.1038/s41591-019-0667-0]
26. Vatanen T, Franzosa EA, Schwager R, Tripathi S, Arthur TD, Vehik K, Lernmark A, Hagopian WA, Rewers MJ, She JX, Toppari J, Ziegler AG, Akolkar B, Krischer JP, Stewart CJ, Ajami NJ, Petrosino JF, Gevers D, Lahdesmaki H, Vlamakis H, Huttenhower C, Xavier RJ. The human gut microbiome in early-onset type 1 diabetes from the TEDDY study. Nature. 2018: 589 [PMID: 30356183 https://doi.org/10.1038/s41586-018-0620-2]
27. Stolarczyk E, Vong CT, Garrido-Mesa N, Marks E, Abdel-Aziz D, Ju Q, Jackson I, Powell N, Lord GM, Howard JK. Global deletion of the immune cell transcription factor, T-bet, alters gut microbiota and insulin sensitivity in mice. Frontiers in genetics. 2024: 1502832 [PMID: 39664730 https://doi.org/10.3389/fgene.2024.1502832]
28. Ismail L, Materwala H, Al Kaabi J. Association of risk factors with type 2 diabetes: A systematic review. Computational and structural biotechnology journal. 2021: 1759 [PMID: 33897980 https://doi.org/10.1016/j.csbj.2021.03.003]
29. Qiu J, Yin W, Wang R, Luo S, Zhou Z. Fulminant type 1 diabetes: Focusing on triggering factors. Diabetes/metabolism research and reviews. 2024: e3731 [PMID: 37814918 https://doi.org/10.1002/dmrr.3731]
30. Golovaty I, Ritchie ND, Tuomilehto J, Mohan V, Ali MK, Gregg EW, Bergman M, Moin T. Two decades of diabetes prevention efforts: A call to innovate and revitalize our approach to lifestyle change. Diabetes research and clinical practice. 2023: 110195 [PMID: 36470316 https://doi.org/10.1016/j.diabres.2022.110195]
31. American Diabetes Association Professional Practice C. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes-2024. Diabetes care. 2024: S145 [PMID: 38078578 https://doi.org/10.2337/dc24-S008]
32. Kahn DJ, Hubbard JL, Dunn S, Hoyt A. Impact of a Nutrition and Diabetes Continuing Education Program on Primary Care Provider's Knowledge, Attitude, and Clinical Practice. Advances in medical education and practice. 2024: 981 [PMID: 39411273 https://doi.org/10.2147/AMEP.S459304]
33. Shubrook JH, Patel M, Young CF. Community-Based Diabetes Awareness Strategy With Detection and Intervention: The Mobile Diabetes Education Center. Clinical diabetes : a publication of the American Diabetes Association. 2024: 125 [PMID: 38230347 https://doi.org/10.2337/cd23-0020]

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Ahmed Y Azzam, Luis Medina Mora, Mahmoud M. Morsy, Muhammed Amir Essibayi, David J. Altschul, Mahmoud Nassar