Abstract
Introduction: Gastrointestinal neuroendocrine carcinomas (GI-NECs) are a diverse group of aggressive tumors with variable clinical outcomes. Although progress has been made in classifying and treating these cancers, detailed real-world data on their anatomical distribution and survival rates are scant. This study utilizes a large database to explore the epidemiological and anatomical distribution patterns and to assess the survival outcomes of GI-NECs.
Methods: We accessed the TriNetX global health research network, comprising about 197 million patient records from 160 healthcare organizations, to perform a retrospective analysis of GI-NEC cases through November 2024. Patients were identified via the ICD-O-3 morphology code 8246/3. We analyzed TNM staging and survival rates across various GI locations.
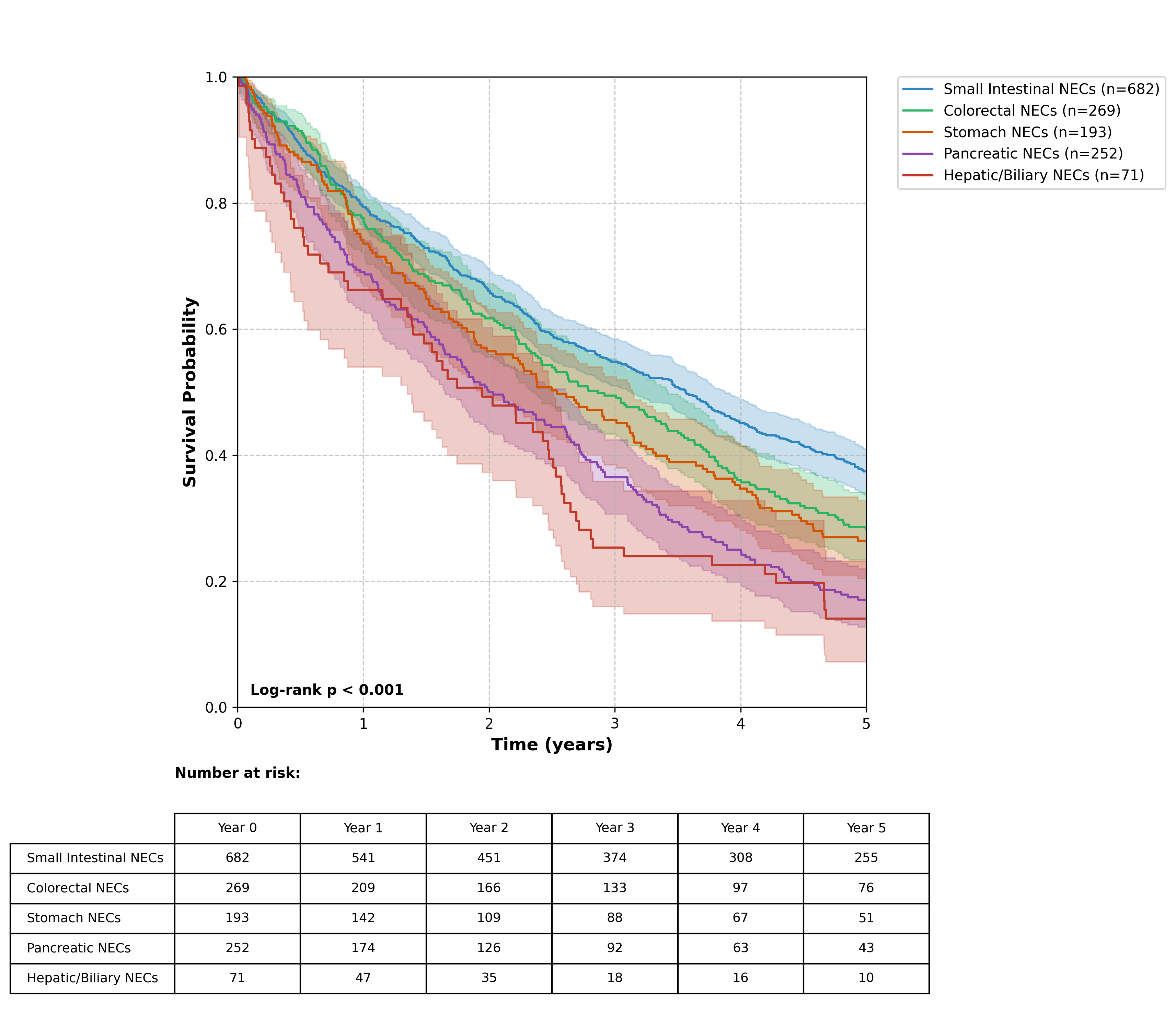
Results: We identified 4,515 cases of NECs with a nearly equal gender distribution (47.27% male, 47.35% female) and an average age of 71 years. Unknown primary sites were the most common (n=692) followed by Small intestinal NECs (n=682) and others. The least common were liver and intrahepatic biliary NECs (n=71). Survival varied significantly by site, from a high of 37.5% in small intestinal NECs to just 11.4% in hepatic/biliary NECs, highlighting notable differences even within the same organ, such as between appendiceal and cecal NECs (44.8% vs. 26.4%).
Conclusions: This study highlights the necessity for site-specific treatment and improved diagnostic strategies, especially for the worst-prognosis NECs found in hepatic and biliary locations. Our findings are vital for developing targeted therapies and refining prognostic tools based on anatomical sites.
References
1. Thiis-Evensen E, Boyar Cetinkaya R. Incidence and prevalence of neuroendocrine neoplasms in Norway 1993-2021. J Neuroendocrinol. 2023: e13264 [PMID: 36988112, https://doi.org/10.1111/jne.13264]
2. White BE, Rous B, Chandrakumaran K, Wong K, Bouvier C, Van Hemelrijck M, George G, Russell B, Srirajaskanthan R, Ramage JK. Incidence and survival of neuroendocrine neoplasia in England 1995-2018: A retrospective, population-based study. Lancet Reg Health Eur. 2022: 100510 [PMID: 36176500, https://doi.org/10.1016/j.lanepe.2022.100510]
3. Alwan H, La Rosa S, Andreas Kopp P, Germann S, Maspoli-Conconi M, Sempoux C, Bulliard JL. Incidence trends of lung and gastroenteropancreatic neuroendocrine neoplasms in Switzerland. Cancer Med. 2020: 9454 [PMID: 33078908, https://doi.org/10.1002/cam4.3524]
4. Rindi G, Klimstra DS, Abedi-Ardekani B, Asa SL, Bosman FT, Brambilla E, Busam KJ, de Krijger RR, Dietel M, El-Naggar AK, Fernandez-Cuesta L, Kloppel G, McCluggage WG, Moch H, Ohgaki H, Rakha EA, Reed NS, Rous BA, Sasano H, Scarpa A, Scoazec JY, Travis WD, Tallini G, Trouillas J, van Krieken JH, Cree IA. A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod Pathol. 2018: 1770 [PMID: 30140036, https://doi.org/10.1038/s41379-018-0110-y]
5. Gill AJ. Why did they change that? Practical implications of the evolving classification of neuroendocrine tumours of the gastrointestinal tract. Histopathology. 2021: 162 [PMID: 33382490, https://doi.org/10.1111/his.14172]
6. Inzani F, Petrone G, Rindi G. The New World Health Organization Classification for Pancreatic Neuroendocrine Neoplasia. Endocrinol Metab Clin North Am. 2018: 463 [PMID: 30098710, https://doi.org/10.1016/j.ecl.2018.04.008]
7. Escobar KM, Vicente-Villardon JL, Villacis Gonzalez RE, Castillo Cordova PH, Sanchez Rodriguez JM, De la Cruz-Velez M, Siteneski A. Neuroendocrine Tumors: An Analysis of Prevalence, Incidence, and Survival in a Hospital-Based Study in Ecuador. Healthcare (Basel). 2022: [PMID: 36011226, https://doi.org/10.3390/healthcare10081569]
8. Helderman NC, Suerink M, Kilinc G, van den Berg JG, Nielsen M, Tesselaar MET. Relation between WHO Classification and Location- and Functionality-Based Classifications of Neuroendocrine Neoplasms of the Digestive Tract. Neuroendocrinology. 2024: 120 [PMID: 37690447, https://doi.org/10.1159/000534035]
9. Palchuk MB, London JW, Perez-Rey D, Drebert ZJ, Winer-Jones JP, Thompson CN, Esposito J, Claerhout B. A global federated real-world data and analytics platform for research. JAMIA Open. 2023: ooad035 [PMID: 37193038, https://doi.org/10.1093/jamiaopen/ooad035]
10. Boyar Cetinkaya R, Aagnes B, Thiis-Evensen E, Tretli S, Bergestuen DS, Hansen S. Trends in Incidence of Neuroendocrine Neoplasms in Norway: A Report of 16,075 Cases from 1993 through 2010. Neuroendocrinology. 2017: 1 [PMID: 26562558, https://doi.org/10.1159/000442207]
11. Koffas A, Giakoustidis A, Papaefthymiou A, Bangeas P, Giakoustidis D, Papadopoulos VN, Toumpanakis C. Diagnostic work-up and advancement in the diagnosis of gastroenteropancreatic neuroendocrine neoplasms. Front Surg. 2023: 1064145 [PMID: 36950054, https://doi.org/10.3389/fsurg.2023.1064145]
12. Merola E, Zandee W, de Mestier L, Klumpen HJ, Makulik K, Geboes K, van Velthuysen ML, Couvelard A, Cros J, van Eeden S, Hoorens A, Stephenson T, Zajecki W, de Herder W, Munir A. Histopathological Revision for Gastroenteropancreatic Neuroendocrine Neoplasms in Expert Centers: Does It Make the Difference? Neuroendocrinology. 2021: 170 [PMID: 32155627, https://doi.org/10.1159/000507082]
13. Lee JE, Hong SH, Jung HI, Son MW, Ahn TS, Han SW, Cho JH. Small-cell neuroendocrine carcinoma of the ileum: case report and literature review. BMC Surg. 2019: 135 [PMID: 31510991, https://doi.org/10.1186/s12893-019-0591-8]
14. Alese OB, Jiang R, Shaib W, Wu C, Akce M, Behera M, El-Rayes BF. High-Grade Gastrointestinal Neuroendocrine Carcinoma Management and Outcomes: A National Cancer Database Study. Oncologist. 2019: 911 [PMID: 30482824, https://doi.org/10.1634/theoncologist.2018-0382]
15. Venizelos A, Elvebakken H, Perren A, Nikolaienko O, Deng W, Lothe IMB, Couvelard A, Hjortland GO, Sundlov A, Svensson J, Garresori H, Kersten C, Hofsli E, Detlefsen S, Krogh M, Sorbye H, Knappskog S. The molecular characteristics of high-grade gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2021: 1 [PMID: 34647903, https://doi.org/10.1530/ERC-21-0152]
16. Burkart J, Owen D, Shah MH, Abdel-Misih SRZ, Roychowdhury S, Wesolowski R, Haraldsdottir S, Reeser JW, Samorodnitsky E, Smith A, Konda B. Targeting BRAF Mutations in High-Grade Neuroendocrine Carcinoma of the Colon. J Natl Compr Canc Netw. 2018: 1035 [PMID: 30181415, https://doi.org/10.6004/jnccn.2018.7043]
17. Chen D, Bao X, Zhang R, Ding Y, Zhang M, Li B, Zhang H, Li X, Tong Z, Liu L, Zhou X, Wang S, Cheng X, Zheng Y, Ruan J, Fang W, Zhao P. Depiction of the genomic and genetic landscape identifies CCL5 as a protective factor in colorectal neuroendocrine carcinoma. Br J Cancer. 2021: 994 [PMID: 34331023, https://doi.org/10.1038/s41416-021-01501-y]
18. Mestre-Alagarda C, Srirajaskanthan R, Zen Y, Giwa M, Howard M, Ooft ML. Genetic and epigenetic prognosticators of neuroendocrine tumours of the GI tract, liver, biliary tract and pancreas: A systematic review and meta-analysis. Histopathology. 2024: 255 [PMID: 37565289, https://doi.org/10.1111/his.15025]
19. Knappskog S, Grob T, Venizelos A, Amstutz U, Hjortland GO, Lothe IM, Kersten C, Hofsli E, Sundlov A, Elvebakken H, Garresori H, Couvelard A, Svensson J, Sorbye H, Perren A. Mutation Spectrum in Liquid Versus Solid Biopsies From Patients With Advanced Gastroenteropancreatic Neuroendocrine Carcinoma. JCO Precis Oncol. 2023: e2200336 [PMID: 36753687, https://doi.org/10.1200/PO.22.00336]

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2024 Bahaaeldin Baraka, Mahmoud Nassar, Ahmed Y. Azzam, Mahmoud M. Morsy, Eyad Ibrahim, Jin Wu, Ahmad Ghorab