Abstract
Introduction: Leukemia and ischemic heart disease (IHD) are major U.S. mortality causes. This study analyzes national mortality trends from 1999 to 2020 to assess the impact of public health efforts in leukemia-associated IHD mortality rates.
Methods: This retrospective study analyzed death certificate data from the CDC-WONDER database spanning 1999 to 2020, focusing on leukemia (ICD-10: C91–C95) and ischemic heart disease (ICD-10: I20–I25) as multiple causes of mortality in the U.S. population. Crude mortality rates (CMR) and age-adjusted mortality rates (AAMR) per 100,000 population were calculated. JoinPoint analysis was performed to estimate annual percent change (APC) and average annual percent change (AAPC).
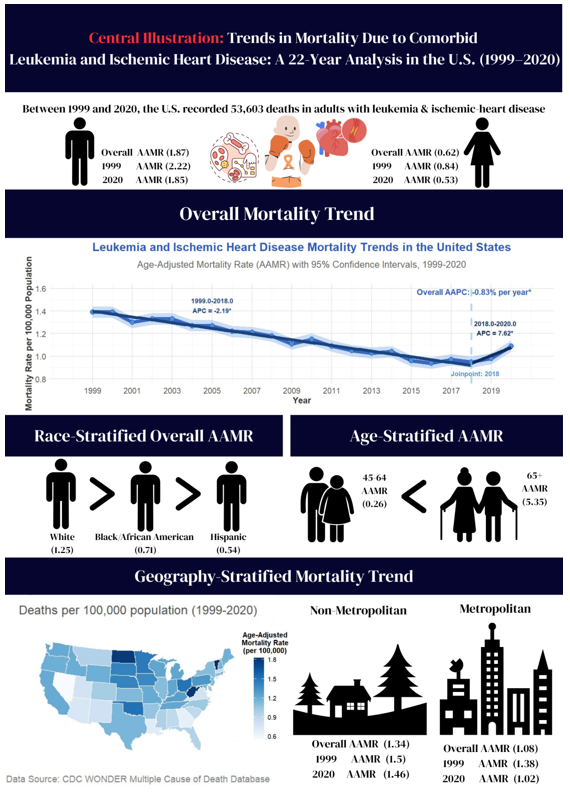
Results: From 1999 to 2020, there were 53,603 deaths from combined leukemia and ischemic heart disease among U.S. adults aged 25+, with the AAMR declining from 1.39 to 1.09 per 100,000 (AAPC= -1.30%; 95% CI: -1.90 to -0.68; P= 0.000034). A significant decrease occurred from 1999 to 2018 (AAMR: 1.39 to 0.95; APC= -2.1894%; 95% CI: -2.3995 to -1.9788, P < 0.000001), followed by a period where the trend shifted upward which is statistically significant for the certain subgroups, except men and older adults. Men had higher AAMR than women (1.87 vs. 0.62). Regional AAMRs were highest in the Midwest (1.3). Non-Hispanic Whites had the highest AAMR (1.25). Adults 65+ had a CMR of 5.27 vs. 0.26 for ages 45–64.
Conclusion: Significant health disparities exist, as mortality from combined leukemia and IHD is highest among men, older adults, rural populations, and non-Hispanic White individuals.
References
1. Okobi OE, Nwogwugwu E, Ihezie CO, Olasupo OO, Emovon CI, Wambai-Sani H, Ezie OB, Afolabi AR, Erinne OC, O'Dare R A. Cardiovascular Disease Patterns, Mortality, and Hospitalization Trends in Adults Over 18: Insights From the Behavioral Risk Factor Surveillance System Database. Cureus. 2024: e66604 [PMID: 39258090, https://doi.org/10.7759/cureus.66604]
2. Dong P, Mao A, Qiu W, Li G. Improvement of Cancer Prevention and Control: Reflection on the Role of Emerging Information Technologies. J Med Internet Res. 2024: e50000 [PMID: 38412009, https://doi.org/10.2196/50000]
3. Asar TO, Ragab M. Leukemia detection and classification using computer-aided diagnosis system with falcon optimization algorithm and deep learning. Sci Rep. 2024: 21755 [PMID: 39294306, https://doi.org/10.1038/s41598-024-72900-3]
4. Ahmed N, Yigit A, Isik Z, Alpkocak A. Identification of Leukemia Subtypes from Microscopic Images Using Convolutional Neural Network. Diagnostics (Basel). 2019: [PMID: 31450720, https://doi.org/10.3390/diagnostics9030104]
5. Aziz N, Nabi W, Khan M, Gulzar AHB, Rath S, Cheema AAA, Arshad MA, Hussain F, Titus A, Lal A, Anwar F. Analyzing Two Decades of Leukemia Mortality in the U.S. (1999-2020). Clin Lymphoma Myeloma Leuk. 2025: e553 [PMID: 40189429, https://doi.org/10.1016/j.clml.2025.03.006]
6. Bi Y, Huang K, Wang M, Jin Y, Zheng ZJ. Global, regional and national burden and quality of care index (QCI) of leukaemia and brain and central nervous system tumours in children and adolescents aged 0-19 years: a systematic analysis of the Global Burden of Disease Study 1990-2019. BMJ Open. 2025: e093397 [PMID: 40122536, https://doi.org/10.1136/bmjopen-2024-093397]
7. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021: 209 [PMID: 33538338, https://doi.org/10.3322/caac.21660]
8. Martin SS, Aday AW, Allen NB, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker-Smith CM, Bansal N, Beaton AZ, Commodore-Mensah Y, Currie ME, Elkind MSV, Fan W, Generoso G, Gibbs BB, Heard DG, Hiremath S, Johansen MC, Kazi DS, Ko D, Leppert MH, Magnani JW, Michos ED, Mussolino ME, Parikh NI, Perman SM, Rezk-Hanna M, Roth GA, Shah NS, Springer MV, St-Onge MP, Thacker EL, Urbut SM, Van Spall HGC, Voeks JH, Whelton SP, Wong ND, Wong SS, Yaffe K, Palaniappan LP, American Heart Association Council on E, Prevention Statistics C, Stroke Statistics C. 2025 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2025: e41 [PMID: 39866113, https://doi.org/10.1161/CIR.0000000000001303]
9. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Ferguson JF, Generoso G, Ho JE, Kalani R, Khan SS, Kissela BM, Knutson KL, Levine DA, Lewis TT, Liu J, Loop MS, Ma J, Mussolino ME, Navaneethan SD, Perak AM, Poudel R, Rezk-Hanna M, Roth GA, Schroeder EB, Shah SH, Thacker EL, VanWagner LB, Virani SS, Voecks JH, Wang NY, Yaffe K, Martin SS. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022: e153 [PMID: 35078371, https://doi.org/10.1161/CIR.0000000000001052]
10. Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker-Smith CM, Beaton AZ, Boehme AK, Buxton AE, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Fugar S, Generoso G, Heard DG, Hiremath S, Ho JE, Kalani R, Kazi DS, Ko D, Levine DA, Liu J, Ma J, Magnani JW, Michos ED, Mussolino ME, Navaneethan SD, Parikh NI, Poudel R, Rezk-Hanna M, Roth GA, Shah NS, St-Onge MP, Thacker EL, Virani SS, Voeks JH, Wang NY, Wong ND, Wong SS, Yaffe K, Martin SS, American Heart Association Council on E, Prevention Statistics C, Stroke Statistics S. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation. 2023: e93 [PMID: 36695182, https://doi.org/10.1161/CIR.0000000000001123]
11. Singh R, Chandi SK, Sran S, Aulakh SK, Nijjar GS, Singh K, Singh S, Tanvir F, Kaur Y, Sandhu APS. Emerging Therapeutic Strategies in Cardiovascular Diseases. Cureus. 2024: e64388 [PMID: 39131016, https://doi.org/10.7759/cureus.64388]
12. Llerena-Velastegui J, Zumbana-Podaneva K, Velastegui-Zurita S, Mejia-Mora M, Perez-Tomassetti J, Cabrera-Cruz A, Haro-Arteaga P, de Jesus A, Coelho PM, Sanahuja-Montiel C. Comparative Efficacy of Percutaneous Coronary Intervention Versus Coronary Artery Bypass Grafting in the Treatment of Ischemic Heart Disease: A Systematic Review and Meta-Analysis of Recent Randomized Controlled Trials. Cardiol Res. 2024: 153 [PMID: 38994227, https://doi.org/10.14740/cr1638]
13. Florek K, Kubler M, Gorka M, Kubler P. New Modifiable Risk Factors Influencing Coronary Artery Disease Severity. Int J Mol Sci. 2024: [PMID: 39063008, https://doi.org/10.3390/ijms25147766]
14. Rouleau CR, Chirico D, Wilton SB, MacDonald MK, Tao T, Arena R, Campbell T, Aggarwal S. Mortality Benefits of Cardiac Rehabilitation in Coronary Artery Disease Are Mediated by Comprehensive Risk Factor Modification: A Retrospective Cohort Study. J Am Heart Assoc. 2024: e033568 [PMID: 38761079, https://doi.org/10.1161/JAHA.123.033568]
15. Abrahams T, Nicholls SJ, Nelson AJ. Optimal Medical Therapy for Stable Ischemic Heart Disease in 2024: Focus on Blood Pressure and Lipids. Med Clin North Am. 2024: 441 [PMID: 38548456, https://doi.org/10.1016/j.mcna.2023.12.005]
16. American Cancer S. Annual cancer facts & figures. American Cancer Society.
17. Li S, Li W, Cheng M, Wang X, Chen W. Prevention and treatment of anthracycline-induced cardiotoxicity: a systematic review and network meta-analysis of randomized controlled trials. Cardiooncology. 2025: 66 [PMID: 40640889, https://doi.org/10.1186/s40959-025-00360-3]
18. Sayegh N, Yirerong J, Agarwal N, Addison D, Fradley M, Cortes J, Weintraub NL, Sayed N, Raval G, Guha A. Cardiovascular Toxicities Associated with Tyrosine Kinase Inhibitors. Curr Cardiol Rep. 2023: 269 [PMID: 36795308, https://doi.org/10.1007/s11886-023-01845-2]
19. Wang H, Wang Y, Li J, He Z, Boswell SA, Chung M, You F, Han S. Three tyrosine kinase inhibitors cause cardiotoxicity by inducing endoplasmic reticulum stress and inflammation in cardiomyocytes. BMC Med. 2023: 147 [PMID: 37069550, https://doi.org/10.1186/s12916-023-02838-2]
20. Chen G, Chen G, Zhou H, Yang Q, Shang Y, Qin R, Hou Y, Zhang C, Lin J, Ye X, Wang N, Feng Y. A bibliometric analysis of targeted therapy cardiotoxicity research in cancer patients (2004-2024). Front Med (Lausanne). 2025: 1593178 [PMID: 40641976, https://doi.org/10.3389/fmed.2025.1593178]
21. Upshaw JN, Nelson J, Rodday AM, Kumar AJ, Klein AK, Konstam MA, Wong JB, Jaffe IZ, Ky B, Friedberg JW, Maurer M, Kent DM, Parsons SK. Association of Preexisting Heart Failure With Outcomes in Older Patients With Diffuse Large B-Cell Lymphoma. JAMA Cardiol. 2023: 453 [PMID: 36988926, https://doi.org/10.1001/jamacardio.2023.0303]
22. Feuchtinger T, Bader P, Subklewe M, Breidenbach M, Willier S, Metzler M, Gokbuget N, Hauer J, Muller F, Schlegel PG, Fruhwald M, Schmid C, Troeger A, Baldus C, Meisel R, Kunkele A, Topp M, Bourquin JP, Cario G, Von Stackelberg A, Peters C. Approaches for bridging therapy prior to chimeric antigen receptor T cells for relapsed/refractory acute lymphoblastic B-lineage leukemia in children and young adults. Haematologica. 2024: 3892 [PMID: 38356450, https://doi.org/10.3324/haematol.2023.283780]
23. National Cancer I. Research areas - cancer disparities. National Cancer Institute.
24. Qu Q, Guo Q, Shi J, Chen Z, Sun J, Cheang I, Gao R, Zhou Y, Zhang H, Liao S, Yao W, Li X. Trends in cardiovascular risk factor prevalence, treatment, and control among US adolescents aged 12 to 19 years, 2001 to March 2020. BMC Med. 2024: 245 [PMID: 38872207, https://doi.org/10.1186/s12916-024-03453-5]
25. Centers for Disease C, Prevention. Centers for Disease Control and Prevention website. CDC.
26. Essa M, Ghajar A, Delago A, Hammond-Haley M, Shalhoub J, Marshall D, Salciccioli JD, Sugeng L, Philips B, Faridi KF. Demographic and State-Level Trends in Mortality Due to Ischemic Heart Disease in the United States from 1999 to 2019. Am J Cardiol. 2022: 1 [PMID: 35317929, https://doi.org/10.1016/j.amjcard.2022.02.016]
27. Chen J, Pang W, Deng M, Zheng R, Chen Y, Zhang Z, Tan Z, Bai Z. Global, regional, and national burden of leukemia, 1990-2021: a systematic analysis of the global burden of disease in 2021. Front Med (Lausanne). 2025: 1542317 [PMID: 40303374, https://doi.org/10.3389/fmed.2025.1542317]
28. Bureau USC. Geographic terms and definitions. U.S. Census Bureau.
29. Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat 2. 2014: 1 [PMID: 24776070,
30. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008: 344 [PMID: 18313558, https://doi.org/10.1016/j.jclinepi.2007.11.008]
31. Doolub G, Raichman A, Abramov D, Bang V, Parwani P, Karunanithi K, Abdel-Qadir H, Kobo O, Mamas MA. Temporal trends in cardiovascular mortality among patients with hematological malignancies: a 20-year perspective. Expert Rev Cardiovasc Ther. 2025: 35 [PMID: 39916300, https://doi.org/10.1080/14779072.2025.2463332]
32. Avery CL, Howard AG, Nichols HB. Trends in US Cancer and Heart Disease Mortality, 1999-2018. Circulation. 2021: 287 [PMID: 33464967, https://doi.org/10.1161/CIRCULATIONAHA.120.051451]
33. Wong N, Vulić D, Šobot M. Implementation of secondary prevention methodologies in ischemic heart disease. Scripta Medica. 2010: 29 https://doi.org/10.5937/ScriMed1001029W]
34. Durugu SR, Ali H, Sinha S, Kalantri S, Ahmed F, Abboud B, Rojulpote KV, Thirumaran R. Trends in Mortality Due to Hematologic Malignancies Among Patients Aged 25 and Older in the United States: Annual Trends and Insights on Gender Disparities from the CDC Wonder Database. Blood. 2024: 7936 https://doi.org/10.1182/blood-2024-206738]
35. Lv Y, Cao X, Yu K, Pu J, Tang Z, Wei N, Wang J, Liu F, Li S. Gender differences in all-cause and cardiovascular mortality among US adults: from NHANES 2005-2018. Front Cardiovasc Med. 2024: 1283132 [PMID: 38420264, https://doi.org/10.3389/fcvm.2024.1283132]
36. Carberry J, Aubiniere-Robb L, Kamdar A, Lomholt-Welch H, Berry C. Reappraising Ischemic Heart Disease in Women. Rev Cardiovasc Med. 2023: 118 [PMID: 39076281, https://doi.org/10.31083/j.rcm2404118]
37. Samad F, Agarwal A, Samad Z. Stable ischemic heart disease in women: current perspectives. Int J Womens Health. 2017: 701 [PMID: 29033611, https://doi.org/10.2147/IJWH.S107372]
38. Ahmed S, Ahmad E, Ashraf H, Ashfaq H, Akram U, Ahmad S. Trends and Disparities in Acute Lymphoblastic Leukemia-Related Mortality in the United States from 1999 to 2020: Insights From the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research Database. Am J Clin Oncol. 2025: 215 [PMID: 39886753, https://doi.org/10.1097/COC.0000000000001162]
39. Howlader N, Sharon E, Bhattacharya M, Ehrlich LA, Richardson NC, Gormley NJ, de Claro RA, Wood AE, Mariotto AB, Cronin KA. The Impact of Improved Treatments on Survival of Adult U.S. Leukemia Patients: 1990-2018. Cancer Epidemiol Biomarkers Prev. 2023: 744 [PMID: 37012203, https://doi.org/10.1158/1055-9965.EPI-22-1171]
40. Rodriguez F, Hastings KG, Boothroyd DB, Echeverria S, Lopez L, Cullen M, Harrington RA, Palaniappan LP. Disaggregation of Cause-Specific Cardiovascular Disease Mortality Among Hispanic Subgroups. JAMA Cardiol. 2017: 240 [PMID: 28114655, https://doi.org/10.1001/jamacardio.2016.4653]
41. Pinheiro PS, Williams M, Miller EA, Easterday S, Moonie S, Trapido EJ. Cancer survival among Latinos and the Hispanic Paradox. Cancer Causes Control. 2011: 553 [PMID: 21279543, https://doi.org/10.1007/s10552-011-9727-6]
42. Downey LH. Rural Populations and Health: Determinants, Disparities, and Solutions. Preventing Chronic Disease. 2013: https://doi.org/10.5888/pcd10.130097]
43. Abdelmalek M, Lee Y-C, Jizzini M, Chang K-Y, Lee Y, Wang ES. Association between the Leukemia Mortality-to-Incidence Ratio and State Geographic Healthcare Disparities in the United States. Blood. 2021: 3066 https://doi.org/10.1182/blood-2021-151798]
44. Markman TM, Markman M. Cardio-Oncology: mechanisms of cardiovascular toxicity. F1000Res. 2018: 113 [PMID: 29399333, https://doi.org/10.12688/f1000research.12598.1]
45. Zhang H, He M, Zhang P, Gao Y, Ouyang L, He X, Han N, Zhang J, Guan M, Feng Y, Li Y. Long-Term Risks of Cardiovascular Death among Older Patients with Major Hematological Malignancies: A Population-Based Cohort Study from SEER Database. Cancer Epidemiol Biomarkers Prev. 2024: 1167 [PMID: 38713156, https://doi.org/10.1158/1055-9965.EPI-23-1635]
46. Ayaz A, Naqvi SA, Farooq S, Sickora K, Wazir MH, Hajj ME, Lateef TS, Masood A, Amin S, Rajkumar C, Patel M, Husnain M, Riaz IB, Mir SA. Cardiovascular (CV) Mortality Among Adults Diagnosed with Leukemias: A Retrospective Cohort Study. Blood. 2023: 2426 https://doi.org/10.1182/blood-2023-190472]
47. Kostakou PM, Kouris NT, Kostopoulos VS, Damaskos DS, Olympios CD. Cardio-oncology: a new and developing sector of research and therapy in the field of cardiology. Heart Fail Rev. 2019: 91 [PMID: 30073443, https://doi.org/10.1007/s10741-018-9731-y]
48. Kanemitsu K, Hassan BD, Mdivnishvili M, Abbas N. The Impact of Lifestyle Intervention Programs on Long-Term Cardiac Event-Free Survival in Patients With Established Coronary Artery Disease. Cureus. 2024: e76585 [PMID: 39881913, https://doi.org/10.7759/cureus.76585]
49. Nalley C. Working in a Rural Setting as a Hematologist/Oncologist. Oncology Times. 2023: 6 https://doi.org/10.1097/01.Cot.0000996460.08434.12]
50. Fatehi F, Taylor M, Caffery LJ, Smith AC. Telemedicine for clinical management of adults in remote and rural areas. In: Atkinson K, Mabey D, editors.: Wiley-Blackwell; 2019. p. 441–461-441–461.
51. Prsic EH, Teno JM, Gozalo P. Site of death, place of care, and burdensome transitions among patients with advanced solid tumor malignancies or leukemia between 2000 and 2010. Journal of Clinical Oncology. 2015: 144 https://doi.org/10.1200/jco.2015.33.29_suppl.144]
52. Shaw B, Parker C, Shortt J, Opat S, Poon P. P1678: Interventions and Therapy at End of Life in Haematological Malignancy: A Retrospective Cohort Study on Healthcare Utilisation. HemaSphere. 2023: https://doi.org/10.1097/01.HS9.0000973584.86598.b8]
53. Mannis GN, McNey LM, Gupta NK, Gross DM. The transfusion tether: Bridging the gap between end-stage hematologic malignancies and optimal end-of-life care. Am J Hematol. 2016: 364 [PMID: 26799788, https://doi.org/10.1002/ajh.24294]
54. LeBlanc TW. Addressing End-of-Life Quality Gaps in Hematologic Cancers: The Importance of Early Concurrent Palliative Care. JAMA Intern Med. 2016: 265 [PMID: 26720324, https://doi.org/10.1001/jamainternmed.2015.6994]
55. Erdal S, Arslan EN, Tandoruk MS. Palliative Care in Patients with Hematological Malignancies. Florence Nightingale J Nurs. 2023: S59 [PMID: 37162056, https://doi.org/10.5152/FNJN.2023.23046]

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2025 Mohamed Fawzi Hemida, Ayesha Khan, Alyaa Ahmed Ibrahim, Anika Goel, Krish Patel, Zahin Shahriar, Ahmed W. Hageen, Mustafa Alsaadi, Saif Ur Rahman, Amr Arafa, Zeyad Kholeif, Ahmed Bahnasy